Dylan Stoll | Health Editor
Featured image courtesy of Pixabay
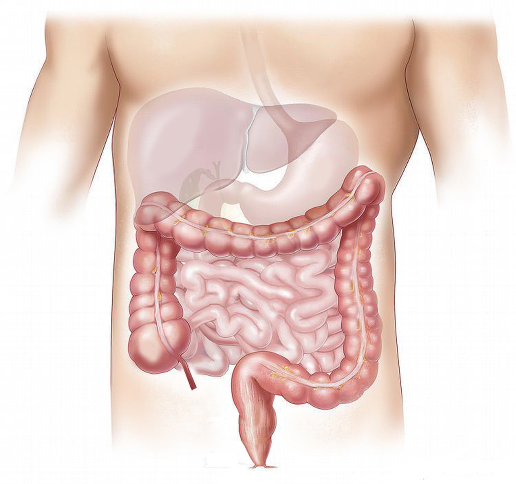
More and more research as of late has been connecting two seemingly disparate organs of the human body: the brain and the stomach.
How, you might ask? Through conditions of the mind such as schizophrenia, depression, anxiety, and even autism.
A study published in Nature looked to elaborate on this connection by beginning with the review of an experiment from 2003 that involved two autistic boys, each with the same single-gene mutation related to autism.
The experiment itself was conducted in an attempt to isolate which genes may be responsible for the condition. In doing so, they also noticed that both boys had diarrhea and esophagitis — gastrointestinal issues (GI) that have been found to be surprisingly common among those with autism.
The correlation between autism and the gastrointestinal tract has been documented many times since then. A review conducted in 2001, for example, established that children with autism were as much as four times as likely to have GI issues than a child without autism.
After reviewing the 2003 study, the researchers completed their own study, but on mice. The researchers genetically altered the mice to have the same single-gene mutation as the boys in the aforementioned study. What resulted were mice with usual autistic behaviours: altered social interactions, repetitive behaviours, communication problems, and yet again, GI incongruities.
Following the breadcrumb trail and taking their experiment even further, they analyzed the microbiota of the mutated mice and discovered that the ratio between two particular types of bacteria, Firmicutes and Bacteroidetes, had been changed. This altered ratio is also evident in people with type 2 diabetes, inflammatory bowel disease and obesity.
Now another study came forth last year illustrating this very same GI tract-autism connection. What they discovered was that up to 90 per cent of autistic people, adults and children, experience consistent GI issues over the course of their life, a condition they’ve attributed to mutations in their genomes.
We know the brain and gut share many of the same neurons and now for the first time we’ve confirmed that they also share autism-related gene mutations,” said Chief Investigator of the study, Associate Professor Elisa Hill-Yardin. “Our findings suggest these gastrointestinal problems may stem from the same mutations in genes that are responsible for brain and behavioural issues in autism.”
As a result of this mutation, what occurs is the “Velcro” between neurons, the substance that keeps them in close contact so as to facilitate efficient communication, becomes dysfunctional. In turn, this also causes the connection as a whole to become dysfunctional, hence the symptoms associated with autism.
This communication error also affects the neural pathways that are connected to the gut. Due to this, the gut experiences changes in gut contractions, the speed at which food moves through the small intestine, and even the number of neurons in the small intestine.
“The link we’ve confirmed suggests a broader mechanism, indicating that the mutations that affect connections between neurons could be behind the gut problems in many patients,” said Hill-Yardin.
“It’s a whole new way of thinking about it — for clinicians, families and researchers — and it broadens our horizons in the search for treatments to improve the quality of life for people with autism.”